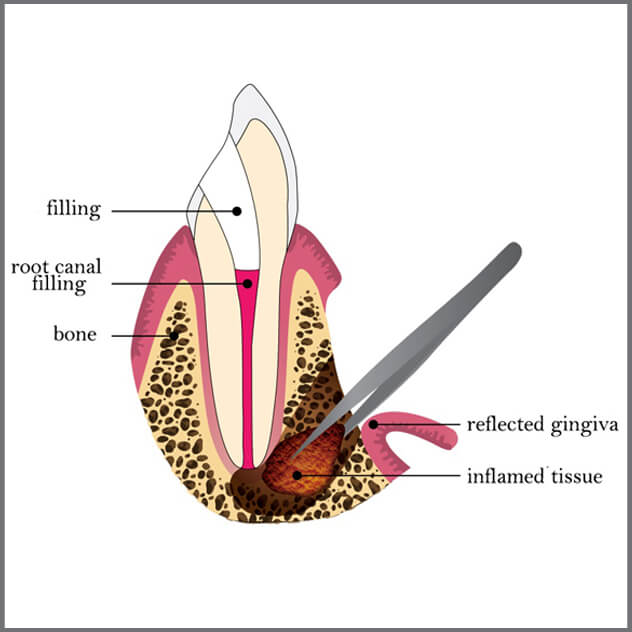
A root canal can fail for several reasons. A tooth can become infected again if your dentist did not completely clean out all of the root canals. Bacteria can get inside a tooth if a filling or crown starts to break down or leak.
A repeat root canal treatment tends to be more involved and take more time than the first one. Your dentist must remove the crown, post and core, and filling material before he or she can do the second root canal. Some people who need another treatment may have infections that are difficult to destroy. Because they take more time and can be complicated, second root canals also usually cost more.
Sometimes a second root canal can be hard to do. For example, it may be too risky to remove a post and core. The post that is in the tooth may be cemented or set in very tightly. If that is the case, the tooth may be injured in the process. So your dentist may decide to do endodontic surgery called apicoectomy instead.
Root Canal Treatment:
Teeth have two basic parts: the crown is the part you see above the gum, and the roots anchor your tooth to your jawbone. Inside the crown and roots is soft tissue (pulp) that helps keep your tooth nourished.
Crown: An outer enamel layer and the dentin inside protect the tooth’s underlying structures and prevent bacteria from entering the tooth.
Root: the root canals house the pulp and extend to the underlying bone. The pulp helps nourish the tooth and is made up of tiny blood vessels and nerves. The blood vessels carry nutrients to the tooth, and the nerves give feeling to the tooth. The bone holds the tooth with the help of tiny ligaments attached to the roots. The pulp tissue enters and exits through openings at the root tips.
How does Endodontic treatment save the tooth?
Root canal or endodontic treatment—treatment done to the inside of the tooth—is necessary when the pulp becomes inflamed or infected. The inflammation or infection can have a variety of causes: deep decay, repeated dental procedures on the tooth, faulty crowns, or a crack or chip in the tooth. In addition, trauma to a tooth may cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
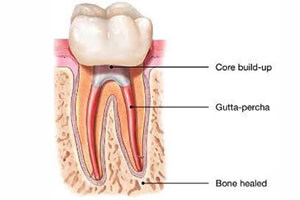
During root canal or endodontic treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called gutta-percha. Afterwards, the tooth is restored with a crown or filling for protection. After restoration, the tooth continues to function like any other tooth.
Endodontic treatment helps you maintain your natural smile and continue eating the foods you love.
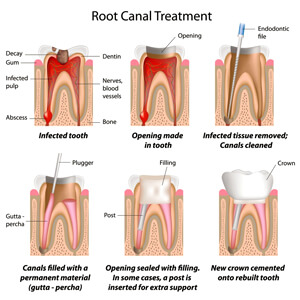
The general sequence of a root canal procedure is as follows:
Step 1
Local anesthesia is administered via injections to numb the tooth to be treated and the surrounding tissues. If the pulp in a tooth is acutely inflamed, and therefore very painful, it may take a while to get it numb, but your dentist will not start the treatment until it is.
Step 2
A small access hole is drilled through the biting surface of an affected back tooth or from behind a front tooth, allowing access to the pulp chamber and root canals for treatment.
Step 3
The diseased and dead pulp tissue is removed from the tooth with specially designed instruments used to clean out the root canals and pulp chamber. This is not painful; the area is numb and the tissue being removed is either dead or dying. Once the pulp, along with the nerves contained in it, is removed, the tooth itself can no longer feel pain.
Step 4
The canals are disinfected with antiseptic and antibacterial solutions.
Step 5
The canals are then shaped with tiny flexible instruments to allow them to receive root canal fillings and sealers. The canals are washed and cleaned again to remove root canal debris prior to sealing them.
Step 6
Root canal fillings are selected that will exactly fit into the freshly prepared canals. Usually a rubber-like material called gutta-percha is used to fill the canal space. It is a thermoplastic material (“thermo” – heat; “plastic” – to shape), which literally is heated and then compressed into and against the walls of the root canals to seal them. Together with adhesive cement called a sealer, the gutta-percha fills the prepared canal space. Sealing the canals is critically important to prevent them from becoming reinfected with bacteria.
Step 7
A temporary or permanent filling material will then be placed to seal the access hole that was made to treat the canals. If the tooth lacks sufficient structure to hold a restoration (filling) in place, the dentist or endodontist may place a post (either metal or a very strong plastic) in one of the canals inside the tooth to help retain it.
Step 8

Root canal filling material (gutta percha) is placed in the canals and the tooth is sealed with a temporary filling to protect it from contamination. Then a crown is usually placed over the tooth to seal and protect it from recontamination and future damage.
After the procedure, an antibiotic may be prescribed to treat or prevent infection. Be sure to follow the instructions of your dentist carefully. After-effects of treatment are minimal, generally lasting from a couple of days to about a week. It is normal to have some minor discomfort after treatment including slight soreness that can usually be managed with over-the-counter (aspirin, ibuprofen) medications or prescription (codeine-type) drugs, or a combination of the two.
Step 9
Your tooth will need a permanent restoration — a filling or a crown — to replace lost tooth structure, and provide a complete seal to the top of the tooth.
Knowledge Is Power
Almost like the root system of a plant, the root canals of a tooth have a main branch and many smaller side branches, and the whole system needs to be sealed during root canal treatment to be successful long term. Since root canals are very small spaces, they require a great deal of precision and care to treat well. Therefore, today we at Perfect Smile Dental Clinic use state-of-the-art technology including radiographic imaging to diagnose root canal problems, and after treatment to verify that the canals are properly sealed; ultrasonic instrumentation to remove old canal fillings and posts and clean canals; and XSmart Endodontic Motor and NiTi Rotary Files to accurately shape, clean and seal root canal systems; it really is quite high-tech.
I have found that people who are nervous tend to lack information about endodontic (root canal) treatment; knowledge gives them the power to understand what’s to come and to eliminate their fears. I hope that this step-by-step explanation will alleviate any apprehension. Root canal treatment really does relieve pain, not cause it — and saves teeth.